Table of Contents
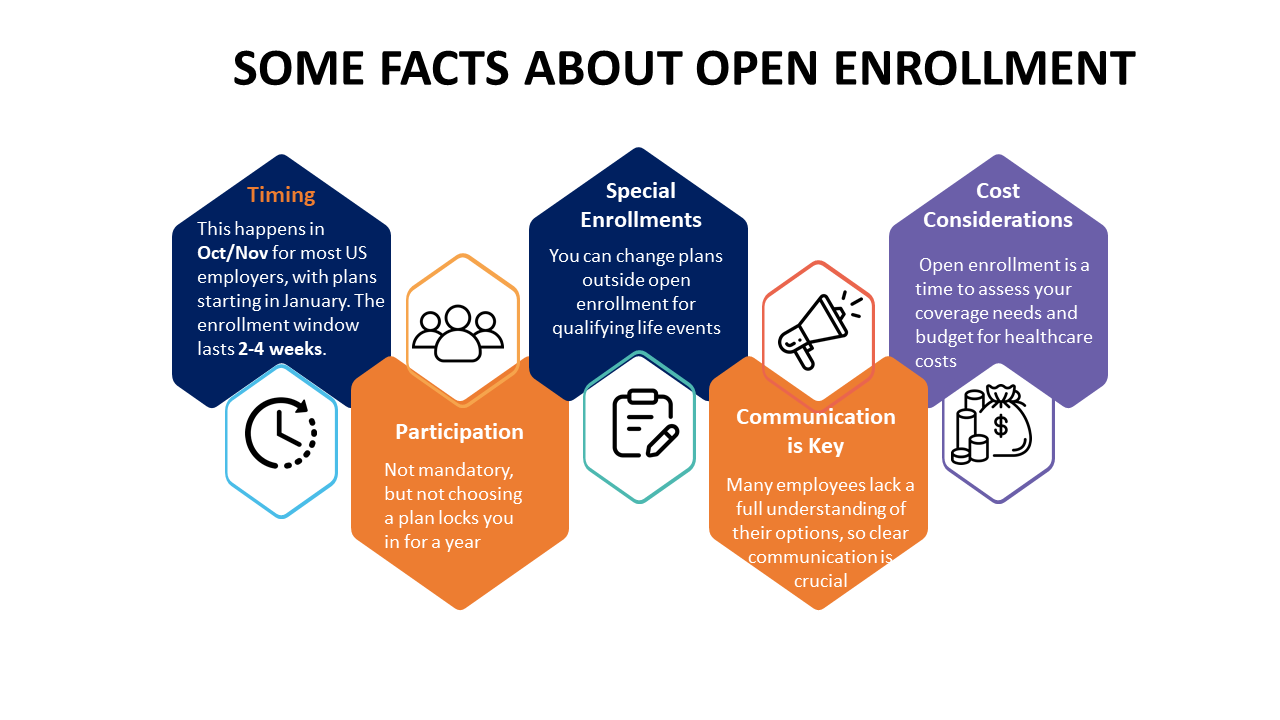
The open enrollment period plays a critical role in benefits administration for organizations and individuals alike. For employees, open enrollment provides an opportunity to review their benefits options and compare costs and coverage levels among different plans. It allows them to make selections that fit their unique needs and priorities. With the right education and assistance from HR and benefits teams, employees can choose open enrollment plans that maximize value. Implementing EDI solutions streamlines benefits enrollment by automating data exchange between employers, insurers, and benefits providers, reducing errors and administrative burdens. EDI solutions enhance efficiency, ensure data accuracy, and simplify the enrollment process for both employees and organizations. Therefore, making the open enrollment process as valuable for employees as it is for the organization should be the goal.
Meanwhile, employers utilize open enrollment solutions to ensure that all eligible staff have access to quality benefits. This will help attract and retain talent in a competitive job market. Employer costs, claims data, and enrollment trends uncovered during open enrollment also help shape future benefits decisions and strategies. When participating in open enrollment, employees and all stakeholders should achieve a mutually beneficial outcome.
The Challenges in the Open Enrollment Process
Many organizations struggle with their benefits enrollment solutions and processes. Common challenges include complex paperwork and forms, limited choices, lack of education and assistance, confusing communications, technical issues, and long waiting times.
Employees often find it difficult to understand their plan options, compare costs and coverage levels, and determine which plans best suit their needs. Some employees miss enrollment deadlines due to complicated processes. On the employer side, open enrollment places significant administrative burdens on HR and benefits teams.
The staff spends considerable time processing paperwork, answering employee questions, and resolving issues. Challenges in benefits communication, documentation, and eligibility verification are common. Employees may become frustrated with the cumbersome enrollment system, resulting in lower participation rates, errors in benefits selections, and reduced satisfaction.
To address these issues, organizations are looking for ways to simplify and automate open enrollment through self-service technologies and streamlined processes. The aim is to make open enrollment more user-friendly for employees while reducing the administrative workload for HR and benefits teams.
Overcoming the Challenges in Open Enrollment Processes
- Adopt self-service technologies: Provide an online enrollment portal where employees can research options, enroll, and make changes on their own time. This reduces paperwork and appointments.
- Offer decision support tools: Use online benefit calculators, health risk assessments, and personalized recommendations to help employees choose the best plans.
- Simplify forms and communications: Use clear, concise language and visual aids to make benefits guides and enrollment forms easy to understand. Limit technical jargon and acronyms.
- Provide on-demand assistance: Offer a contact center, online chat, FAQs and other help resources employees can access anytime. This ensures employees have a way to get their questions answered quickly.
- Improve system reliability: Test new systems thoroughly before implementation and have workarounds in place for any outages. Keeps the system running smoothly during peak enrollment times?
- Align enrollment with payroll: Utilize payroll data for accurate and timely eligibility information. Integrate benefits selections with payroll deductions for a seamless process.
- Enforce deadlines and procedures: Communicate enrollment timelines and requirements to employees. Have protocols in place for employees who miss deadlines.
- Evaluate each enrollment period: Survey employees for feedback. Analyze metrics like enrollment times and error rates. Identify opportunities for further improvements and efficiencies.
By implementing the above strategies as part of open enrollment solutions, organizations can overcome many open enrollment pitfalls and make the experience less stressful for both employees and HR teams.
Best Practices from Successful Open Enrollment Processes
- Provide a user-friendly online portal: Allow employees to enroll, view benefits information, and manage their selections from any device at any time.
- Offer decision support tools: Calculators, personalized recommendations, and educational content can help employees choose the right benefits for their needs.
- Simplify communications: Use clear, concise language and visual aids. Avoid jargon and acronyms. Tailor messaging for specific employee groups.
- Offer multiple education channels: Provide in-person meetings, webinars, videos, on-demand resources, and a contact center for live assistance.
- Enforce deadlines: Communicate enrollment deadlines and requirements to employees. Have policies for late enrollments.
- Integrate technology systems: Link enrollment systems with payroll, HRIS, and any internal portals for a seamless workflow and accurate data.
- Evaluate feedback regularly: Survey employees after each enrollment period. Analyze metrics to identify issues and opportunities for improvement.
- Test systems thoroughly: Pilot new technologies and processes on a small scale before implementing them organization-wide. Have contingencies in place for issues.
- Automate repetitive tasks: Use technologies to automate tasks like verifying employee eligibility and enrollment data. This frees up staff for value-added work.
Common Mistakes to Avoid in Open Enrollment Processes
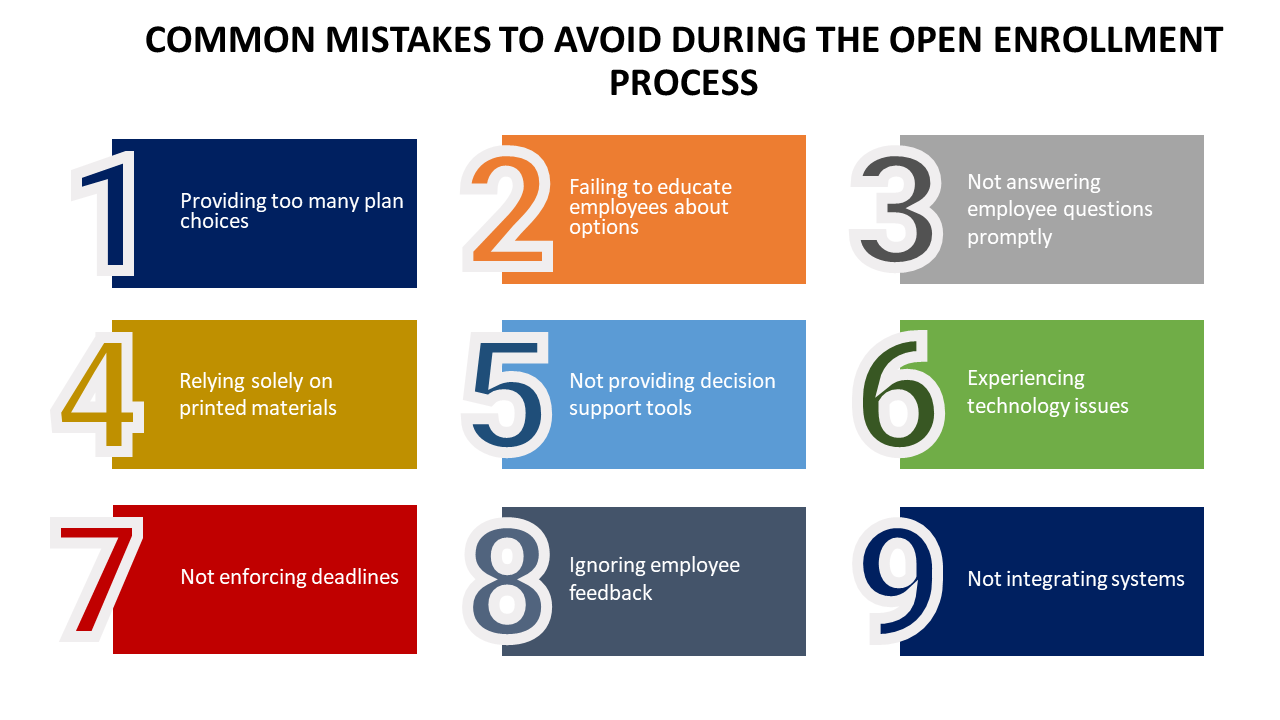
Some of the common mistakes that can affect the ability of an organization to achieve the full potential of open enrollment solutions are as follows-
- Providing too many plan choices: Limit options to the most needed or popular. Too many choices can confuse and overwhelm employees.
- Failing to educate employees about options: Employees can’t make informed decisions without proper information about available plans.
- Not answering employee questions promptly: Delayed responses frustrate employees and reduce satisfaction.
- Relying solely on printed materials: Supplement brochures and booklets with online materials, webinars, and a contact center.
- Not providing decision support tools: Calculators, comparisons, and personalized recommendations help employees choose suitable plans.
- Experiencing technology issues: Test systems thoroughly before enrollment starts and have contingencies for any outages or glitches.
- Not enforcing deadlines: Communicate deadlines and have procedures for late enrollments.
- Ignoring employee feedback: Regularly survey employees to identify pain points, confusion, and opportunities for improvement.
- Not integrating systems: Link enrollment, payroll, and HRIS systems for an efficient, accurate process.
Ensure employee satisfaction and organizational success with our open enrollment solutions
Compliance and Legal Considerations in Open Enrollment Processes
The open enrollment process must comply with various laws and regulations to minimize legal risks. Organizations must ensure all employees have equal access to enroll in benefits and cannot exclude any groups. Required notices and disclosures must be distributed, including summaries of benefits, COBRA notices, and HIPAA privacy notices. Employers must verify that dependents meet eligibility requirements to avoid paying ineligible claims and closely monitor compliance with annual and lifetime limits under the Affordable Care Act. All enrollment information should be documented and stored for the periods required by law.
Proper consent must be obtained to disclose any personal employee information as needed. Employees with disabilities must be provided auxiliary aids, alternative formats, and other accommodations during open enrollment. Health plans themselves must comply with provisions around essential health benefits, out-of-pocket maximums, and other ACA mandates. Legal counsel should be consulted as needed to review enrollment materials, communications, and procedures to minimize compliance risks. Documentation should be maintained of compliance training, policies, procedures, and system controls related to open enrollment.
Evaluating the Success of Open Enrollment Process
Gather feedback from employees through surveys and focus groups. Ask questions to understand pain points, difficulties, sources of confusion, and any issues encountered. Employees can also suggest improvements.
Review data and metrics like completion times, error rates, call volumes, and drop-off rates at various stages of the process. Compare historical data to spot positive or negative trends.
Analyze enrollment selections to determine if plans are meeting employee needs based on plan usage and changes made during special enrollment periods. Look for opportunities to refine plans and communications.
Look at participation and eligibility rates to see if the number of eligible employees enrolling matches targets. Low rates may signal issues requiring attention.
Monitor attrition rates before and after open enrollment to determine if benefit changes are impacting retention. Unexpected changes may require refinement.
Evaluate feedback and input from HR, benefits, and IT teams responsible for administering the process. Staff perspectives on workload, pain points, and sources of confusion can reveal opportunities for automation and simplification.
Consult with legal and compliance teams to ensure all requirements were met and identify any gaps to address for the following year. Verify the accuracy of dependent verifications.
Leveraging Technology for a Smooth Enrollment Process in Open Enrollment Process
Organizations can leverage several technologies to improve the open enrollment process for employees and HR teams. Online enrollment portals allow employees to enroll, modify benefits, and view information from any device at any time. This self-service model reduces paperwork and appointments. Decision support tools like benefit calculators and personalized recommendations help employees choose suitable plans that align with their priorities. Automation of routine tasks through technologies frees up staff time for more strategic duties.
Integrating enrollment systems with payroll, HRIS, and internal portals allows for more seamless data sharing and accurate processing. Online communication channels and virtual education options supplement traditional materials and in-person meetings to better accommodate distributed workforces. Technologies also provide analytics that reveals actionable insights into enrollment trends, issues, and opportunities for improvement. While no technology is a silver bullet, when paired with proper training, support, and process improvements, technologies can streamline and simplify open enrollment.
The focus should remain on how technology can best enhance the user experience for employees. It should also reduce administrative burdens for HR and benefits teams through increased automation, data accuracy, and insight. With the right organizational change management, technologies can help make open enrollment a more efficient and effective process for all involved.
Collaboration between HR and Benefits Teams in open enrollment process
Collaboration between HR and benefits teams is essential for a successful open enrollment process. HR teams focus on the employee experience; ensuring employees have the information and resources needed to choose the right benefits for their needs. They communicate benefit options, eligibility requirements, and deadlines to employees.
Benefits teams focus on managing benefit plans, vendors, and costs. They determine which plans to offer, negotiate with carriers, and analyze utilization data. During open enrollment, both teams work together to verify dependent eligibility, resolve employee questions, troubleshoot issues, and ensure compliance with regulations.
Effective communication and data sharing is critical, with HR teams providing employee records and payroll data to benefits teams and benefits teams updating HR systems with new enrollments and changes. After open enrollment, HR can provide feedback benefits on employee satisfaction and pain points to guide plan decisions. Benefits can share enrollment metrics, plan usage analytics, and cost projections with HR to aid planning and budgeting. Regular meetings throughout the year keep both teams in sync on benefits-related matters impacting employees.
Together, HR and benefits form a united front to simplify and improve the employee experience, optimize the value of benefits programs, and meet organizational talent objectives. By collaborating at each stage of the benefits lifecycle, HR and benefits teams can create an enrollment process that promotes employee engagement, satisfaction, and retention.
Addressing Employee Questions and Concerns in the Open Enrollment Process
Organizations must be prepared to address a variety of employee questions and concerns during open enrollment. Employees may have questions about plan changes, premium costs, network changes, coverage details, dependent eligibility, and documentation requirements. They may be weighing trade-offs between plans with different coverage levels, deductibles, out-of-pocket maximums, and provider networks. Many employees value tools and resources that help them determine which plan best fits their individual needs and budgets.
Organizations should provide multiple channels for employees to get the information and assistance they require. These may include in-person meetings, online resources like FAQs and videos, benefits guides, one-on-one consultations and call centers with trained specialists. Representatives assisting employees must be well-versed in all benefits options and prepared to explain features in clear, easy-to-understand terms. Organizations should strive for prompt responses to employee questions to minimize anxiety and frustration.
After open enrollment ends, benefits teams should analyze the most common questions and concerns to identify themes that could guide improvements for future periods. The goal is to anticipate employee needs, arm representatives with the right knowledge, and provide self-service resources that minimize the need for direct assistance. Organizations can foster a productive dialogue with employees that results in well-informed benefits selections aligned with individual priorities. This can be achieved with clear communication, ample education, and a commitment to continuous improvement.
Open Enrollment and Remote Workforce
With more employees working remotely, organizations must adapt the open enrollment process to accommodate a distributed workforce. While some aspects of open enrollment may remain the same for remote and in-office employees, organizations should consider additional options to ensure all employees have access to information and support.
Online enrollment portals allow remote employees to enroll, change benefits, and access information wherever they are working. Virtual education channels like webinars, videos, and phone consultations reach remote employees who cannot attend in-person meetings. Around-the-clock assistance via contact centers, chatbots, email, and FAQs helps employees get the help they need on their schedule. Organizations should test technology systems ahead of time to ensure remote access works smoothly.
Communication plans for remote employees may require more repetition across multiple channels to accommodate varied schedules. Virtual social events can foster connection and engagement around benefits.
Remote flexibility can reduce barriers to participation for employees balancing work with caregiving duties, second jobs, or other priorities. But lower in-person interaction may also result in more errors and questions.
It requires a shift in organizations’ approach, from focusing on in-person meetings and printed materials distributed at the workplace to incorporating virtual and on-demand options. When the open enrollment process effectively supports remote workforces, organizations can leverage flexibility to improve participation and satisfaction.
Are you ready for Open enrollment?
Contact A3Logics, a benefits enrollment company to get started with the open enrollment planning and implementation
The Role of Managers and Supervisors in the Open Enrollment Process
Managers and supervisors play an important role in helping employees understand and select benefits during open enrollment. While HR and benefits teams own the administration of open enrollment, managers have day-to-day relationships with employees that position them to provide guidance and support.
During open enrollment, managers should communicate deadlines and resources to employees. They should encourage participation, emphasize the value of benefits to health and wellbeing, and be available to answer basic questions. Managers can direct employees to HR, benefits specialists, or decision support tools for more complex inquiries.
Some organizations provide training and materials for managers to aid employee conversations about benefits and coverage options. Managers may review enrollment selections with employees to catch any errors or ask clarifying questions. However, managers should refrain from recommending specific plans and refer employees to educational resources to make independent choices.
After open enrollment, managers remain a source of support for employees as they utilize their benefits. Managers can keep an eye out for indications of issues and direct employees to the proper channels for resolution. While managers do not replace HR and benefits specialists, their role as trusted advisors positioned close to employee needs complements the work of central benefits teams. Managers can reinforce key messages, spot potential issues, and ensure employees get the individualized attention needed to make confident selections.
Trends and innovations in the open enrollment process
- Self-service online enrollment is becoming the norm, allowing employees to enroll and make changes from any device at any time. This convenience improves participation rates and employee satisfaction.
- Decision support tools like calculators, comparisons, and personalized recommendations are increasingly common to help employees select plans that match their needs. These tools promote well-informed benefits selections.
- Virtual education options like webinars, videos, and chatbots are supplementing traditional in-person meetings to reach remote and field-based employees more effectively. These channels help improve education and reduce administrative workloads.
- Data and technology integration is advancing to provide actionable insights into enrollment trends identify sources of confusion and recommend process improvements. Analytics can optimize both the employee experience and HR efficiencies.
Simplified, mobile-friendly enrollment forms and materials are being designed to improve the user experience and reduce administrative work like dependent verifications. Streamlining processes promotes accuracy and timely enrollment.
As the workforce continues to virtualize, technologies are emerging to recreate some of the personalized support of in-person meetings online through interactive chats, videos, and other tools. These innovations in open enrollment aim to maintain human connections that drive employee engagement.
Overall, the above trends indicate open enrollment process is evolving to be more employee-centric, intuitive, and efficient. Continuous improvement relies on technologies, processes, and strategies that make benefit selection easier for employees while reducing workloads for HR teams.
The potential impact of technology advancements on the open enrollment process
Advancing technologies have the potential to significantly impact the open enrollment process. Technologies offer opportunities to make open enrollment more intuitive, personalized, and efficient. These technologies include artificial intelligence, machine learning, advanced data analytics, and automation.
Chatbots and virtual assistants using AI and natural language processing could provide initial assistance to employees without the need for call centers or staff intervention. These tools could route complex questions to specialists while answering basic inquiries automatically.
Advanced analytics and machine learning applied to enrollment data could reveal patterns to predict employee needs, guide plan choices, and proactively recommend changes. Analysis of dependent data could identify ineligible dependents and flag errors automatically.
Automation of routine tasks through RPA bots, AI, and predictive algorithms could reduce the manual workload for benefits staff. Automated processes could verify employee eligibility, confirm coverage selections, and allocate premiums.
Employees could receive personalized benefit recommendations and educational content tailored to their health risks, family situations, and financial priorities. Interactive decision support tools could provide real-time feedback on coverage levels, out-of-pocket costs, and provider choices.
Conclusion
Open enrollment season provides important benefits for both employees and employers. It allows employees to evaluate their coverage needs, compare options, and select plans that align with their priorities and budgets. With adequate education and support, employees can make choices that best serve their health and financial goals. For employers, open enrollment periods ensure all eligible staff have access to quality benefits that help attract and retain talent. Employers also utilize open enrollment data to evaluate the utilization, claims costs, and risks that impact future benefits strategies and planning. When the open enrollment process is effective for both employees and employers, organizations see results in the form of higher staff engagement, satisfaction, and productivity.