The healthcare landscape is witnessing immense transformation and all thanks to the infusion of advanced technologies. One of the biggest implementations here has been of EDI in medical billing. This has made the process of interaction easier between the service providers, payers, and patients. With the help of EDI or Electronic Data Interchange, modern approaches to billing have become more secure and standardized.
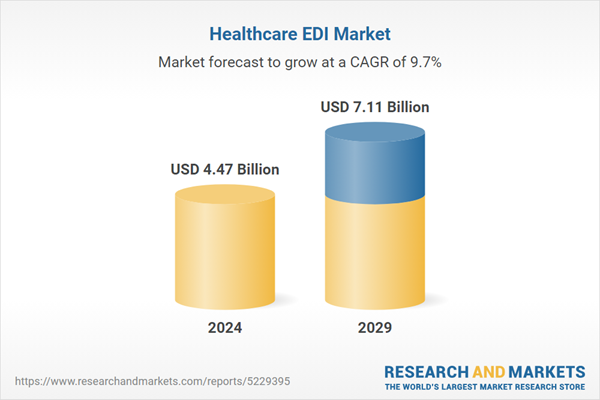
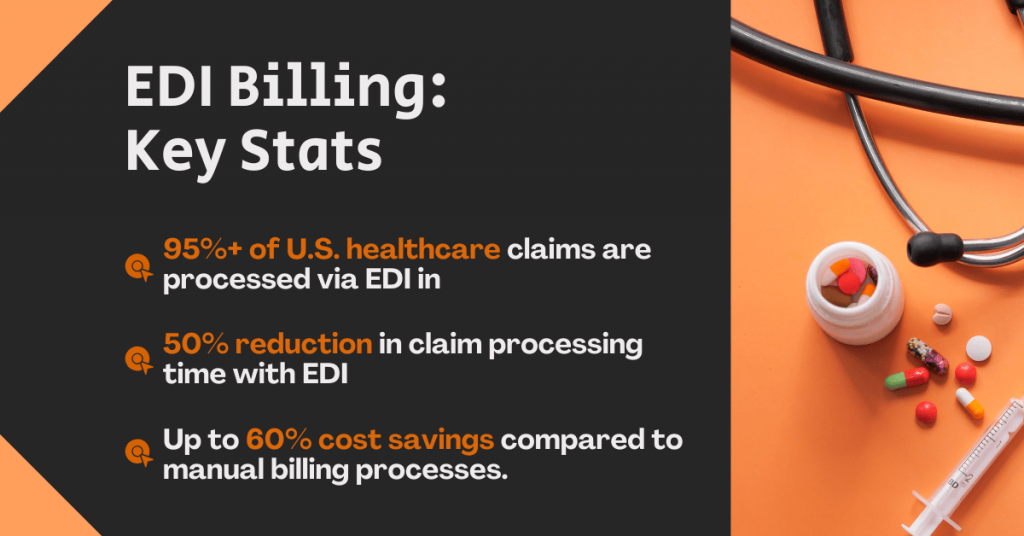
EDI in medical billing automates every aspect of billing without compromising essential healthcare data. This is why more than 95% of the healthcare service providers are now processing electronically with the use of EDI billing software. As the demand is increasing, the global healthcare EDI market is expected to cross $4 billion by the year 2027.
So, if you are thinking about investing in the same, then we have compiled all the information that you need to know about EDI in medical billing.
Table of Contents
EDI Billing: Overview
Using defined digital formats, EDI Billing is the electronic transfer of billing-related data between payers and healthcare providers. From claim filing to remittance advice and payment transfers, it covers the whole billing lifecycle. EDI Billing Software speeds up reimbursements, cuts down on paperwork, and automates these procedures, hence lowering mistakes.
Now that you know what is EDI billing, let’s proceed ahead and understand how medical billing will be affected with the infusion of EDI in the process.
What is EDI in Medical Billing?
EDI in Medical Billing is the application of Electronic Data Interchange to automate the movement of billing information, including claims, eligibility checks, and payment details, between healthcare providers and insurance companies.
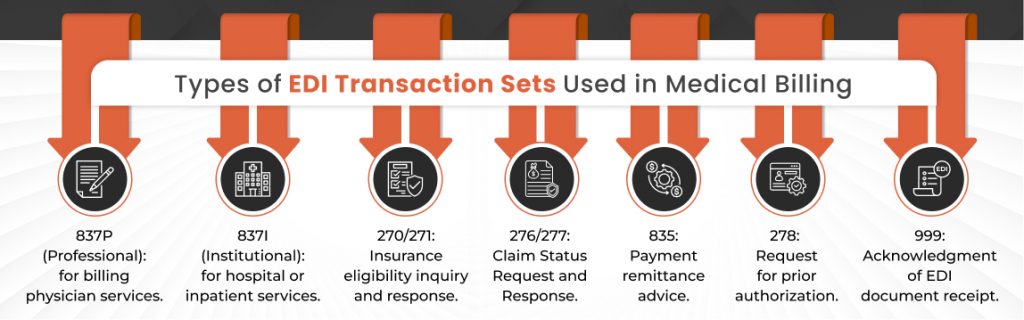
The aim is to simplify the billing procedure, guarantee data correctness, and follow legal requirements including HIPAA. Covering a broad spectrum of transactions, EDI Medical Billing includes benefit enrollment (EDI 834 Services), eligibility questions (EDI 270/271), remittance advice (EDI 835), and claim submissions (EDI 837).
What is EDI Enrollment in Medical Billing?
EDI Enrollment in Medical Billing is how healthcare providers sign up with payers to file claims and get payments sent electronically. Activating EDI Services depends on this enrollment; it lets providers utilize EDI Billing Software for smooth claim submissions, EDI Payments, and real-time claim status checks. Specifically for benefit enrollment and management, EDI 834 Services guarantee that patient coverage information is always current.
How Does EDI Work in Medical Billing?
In this section, we have specified the essential steps that show how EDI works in the Medical Billing domain to enhance efficiency and accuracy.
1. Data Integration
Patient and billing data are gathered from Electronic Health Records (EHR) and practice management systems, then integrated into EDI Billing Software. This step digitizes patient demographics, diagnoses, and treatment details, ensuring seamless data flow while eliminating manual entry errors and redundancies.
2. Claim Creation and Formatting
Claims are generated in standardized EDI formats like ANSI X12 837, which structures clinical and billing data into payer-compliant formats. EDI Billing Software automates this process, ensuring HIPAA adherence and reducing discrepancies that could lead to claim denials or delays.
3. Transmission through a Clearinghouse
Claims are routed through a clearinghouse, which validates, edits, and formats them for specific payer requirements. The clearinghouse acts as a secure intermediary, flagging errors like incorrect codes or missing data before forwarding claims to insurance companies.
4. Payer Processing
Payers use EDI-capable systems to review claims for eligibility, coding accuracy, and coverage. Automated adjudication speeds up approvals or denials, reducing processing time from weeks to days. Denials are flagged with reasons, enabling providers to address issues promptly.
5. Remittance Advice
Payers send electronic remittance advice (EDI 835) detailing paid, denied, or adjusted claims. Providers use this to reconcile payments, identify denials, and update patient billing records, ensuring transparency and reducing follow-up efforts.
6. Claim Status Inquiry
Providers use EDI in Billing to check real-time claim status via EDI 276/277 transactions. This eliminates manual follow-ups by offering instant updates on whether a claim is pending, paid, or denied, directly within the EDI Billing Software.
7. Payment Transfers
Approved payments are transferred electronically via EDI Payments, which directly deposit funds into the provider’s account. This automation accelerates cash flow, reduces administrative delays, and ensures timely reimbursements.
Every single step in the EDI Medical Billing workflow enhances accuracy, speed, and compliance, transforming how healthcare providers manage revenue cycles.
EDI in Medical Billing: Key Components
Below are the key components of EDI in medical billing you must know about to benefit significantly.
1. EDI Billing Software/Gateway
EDI Billing Software or gateway serves as the central hub for automating claim submission, converting data into standardized EDI formats, and securely transmitting information between healthcare providers and payers. This software streamlines the entire billing workflow, reducing manual intervention and minimizing errors. By integrating with Electronic Health Records (EHR) and practice management systems, it ensures that all relevant patient and billing data are accurately captured and formatted. The automation provided by EDI Billing Software allows providers to manage high volumes of claims efficiently, track claim statuses in real time, and accelerate the reimbursement process.
2. Clearinghouse
A clearinghouse acts as a trusted intermediary between healthcare providers and insurance payers. Its primary function is to validate, edit, and route claims to the appropriate payer, ensuring each claim meets specific payer requirements and regulatory standards. The clearinghouse checks for errors, missing information, and formatting issues before forwarding the claim, significantly reducing the risk of rejections or denials.
By providing this layer of quality control, the clearinghouse helps healthcare organizations maintain compliance, improve claim acceptance rates, and streamline communication with multiple payers through a single, unified platform.
3. Standardized EDI Formats
Standardized EDI formats such as ANSI X12 837 (claims), 835 (remittance advice), 834 (benefit enrollment), and 270/271 (eligibility inquiries and responses) are essential for ensuring data consistency and interoperability across the healthcare ecosystem.
These formats provide a structured way to represent complex healthcare transactions, enabling seamless data exchange between providers, payers, and other entities. Healthcare organizations adhere to these standards to reduce misunderstandings, eliminate manual data re-entry, and ensure all parties consistently interpret information, supporting efficient and accurate billing processes.
4. Secure Communication Protocols
EDI-capable systems rely on robust encryption and secure communication protocols to protect sensitive health information during electronic transmission. These protocols ensure that data remains confidential and unaltered as it moves between providers, clearinghouses, and payers. Compliance with regulations such as HIPAA is achieved through the use of secure channels, digital signatures, and authentication mechanisms. This focus on security not only safeguards patient privacy but also builds trust among stakeholders, reduces the risk of data breaches, and supports the overall integrity of the medical billing process.
Benefits of Using EDI in Medical Billing
EDI in Medical Billing significantly increases efficiency and speed by automating repetitive tasks, reducing claim processing times by up to 50%. It reduces errors by eliminating manual data entry mistakes, which minimizes claim denials and rework. Cost savings are substantial, cutting down on paper, postage, and administrative overhead by up to 60%.
Quicker EDI payments enable faster reimbursement cycles, improving cash flow for providers. Standardized data formats improve accuracy by ensuring precise and consistent information exchange.
Enhanced security is provided by EDI-capable systems that use encryption and authentication to safeguard data.
Real-time information access allows instant eligibility checks and claim status updates, streamlining decision-making. Overall, EDI Automation in Healthcare creates a streamlined workflow that integrates seamlessly with existing systems, boosting productivity.
EDI vs Manual Billing: Which is More Efficient?
When comparing EDI in Medical Billing to manual billing, the differences are stark. EDI processes claims within hours or days, while manual billing can take days or even weeks.
The error rate with EDI is very low due to automated validation, whereas manual billing is prone to human error. Costs associated with EDI are lower because it minimizes paper, postage, and labor expenses, while manual billing incurs higher overhead.
Security is stronger with EDI because of encrypted, HIPAA-compliant transmissions, whereas manual billing risks lost or mishandled documents. Real-time status updates are available with EDI, but manual billing often suffers from delays.
Lastly, EDI is highly scalable and can handle large volumes easily, unlike manual billing which is limited by staff capacity. Clearly, EDI in Medical Billing is the more efficient and reliable choice.
Best EDI Billing Software Development Companies for Healthcare Providers
If you are looking for experts to help you with EDI billing software development services, then below are the top names in the business. Check it out.
1. A3Logics

A3Logics is a leading provider of custom EDI Billing Software and EDI Services for healthcare organizations of all sizes. The company specializes in tailored EDI Medical Billing solutions, EDI Automation in Healthcare, and end-to-end EDI Consulting Services.
Their expertise includes developing EDI Capable platforms that integrate with existing systems, streamline claims processing, and ensure compliance with industry standards. A3Logics also supports EDI 834 Services and advanced EDI Payments, making them a trusted partner for efficient, secure, and scalable EDI in Medical Billing.
2. Availity

Availity is a prominent name in EDI Medical Billing, offering a robust platform that connects over a million providers with thousands of payers nationwide. Their EDI Billing Software enables real-time eligibility checks, claim submissions, payment status tracking, and electronic remittance advice. Availity’s EDI Services focus on reducing denials, expediting EDI Payments, and improving collaboration between payers and providers. Their solutions also support EDI Automation in Healthcare, making revenue cycle management seamless and efficient for practices of all sizes.
3. Kareo

Kareo is recognized for its user-friendly EDI Billing Software, specifically designed for small to mid-sized healthcare practices. The platform simplifies EDI in Billing by automating claim creation, submission, and tracking, while integrating with electronic health records and practice management systems. Kareo’s EDI Medical Billing solutions help providers reduce administrative burden, minimize errors, and accelerate EDI Payments. Their intuitive interface and dedicated support make it easy for practices to adopt EDI Automation in Healthcare without extensive technical expertise.
4. Waystar

Waystar delivers advanced EDI Services and analytics for healthcare revenue cycle management. Their EDI Billing Software is known for its powerful automation features, including claim scrubbing, denial management, and real-time reporting. Waystar’s platform is EDI Capable and integrates with a wide range of EHRs and billing systems, supporting EDI Payments and EDI 834 Services. The company’s focus on data-driven insights and workflow optimization helps providers maximize reimbursement and maintain compliance with industry standards.
5. Change Healthcare

Change Healthcare is an industry leader in EDI Capable platforms and comprehensive EDI Consulting Services. Their EDI Billing Software supports high-volume claims processing, advanced EDI Automation in Healthcare, and seamless integration with provider and payer systems.
Change Healthcare’s solutions include EDI 834 Services, electronic remittance, and secure EDI Payments, making them a preferred choice for large healthcare organizations. Their expertise ensures efficient, compliant, and future-ready billing operations.
Difference Between EDI Billing and EDI Invoicing
Although often confused, EDI Billing and EDI Invoicing serve different functions. EDI Billing refers to the entire electronic exchange related to billing, including claims submission, remittance advice, and payment transfers.
EDI Invoicing, on the other hand, specifically involves the electronic exchange of invoices, such as the ANSI X12 810 transaction set. While invoicing is a component of billing, EDI Billing covers a broader spectrum of transactions within the healthcare revenue cycle.
So, understanding this distinction helps healthcare organizations implement more comprehensive and effective EDI Medical Billing strategies.
What’s the Future of EDI in Medical Billing?
The future of EDI in Medical Billing is bright and dynamic. Greater EDI Automation in Healthcare will leverage artificial intelligence and machine learning to reduce manual intervention and speed up claim adjudication.
Interoperability will improve as EDI Billing Software integrates more deeply with Electronic Health Records (EHRs) and payer systems. The adoption of EDI 834 Services for enrollment and maintenance will expand, along with real-time EDI Payments that enhance financial workflows.
Cloud-based EDI Capable solutions will become more prevalent, offering scalable, secure, and accessible platforms. Additionally, regulatory compliance will continue to evolve, requiring ongoing updates to meet HIPAA and industry standards. These advancements will further streamline medical billing and improve healthcare outcomes.
Partner with A3Logics for EDI Medical Billing Consulting
A3Logics, a leading provider of EDI Consulting Services, provides customized solutions for EDI Medical Billing, EDI Billing Software development, and smooth EDI Automation in Healthcare. Their knowledgeable staff guarantees your company becomes completely EDI Capable, compliant, and ready to use the newest EDI Services, including EDI 834 Services and EDI Payments, for optimum operational efficiency and financial performance.
Final Thought
Hopefully you have got complete clarity about how EDI in Medical Billing is no longer just an option. It is one of the most important aspects for healthcare providers who are thinking about streamlining their operations while reducing expenses. With the help of EDI implementation, not only these objectives are ticked but also the healthcare providers are able to deliver better patient care.